In 2021, nearly 1 in 4 Canadian healthcare workers faced harassment or threats while working. This sparked quick legal action to protect medical staff. Ensuring healthcare access became crucial after protests against vaccination policies.
On December 17, 2021, Bill C-3 got Royal Assent. It changed the Criminal Code to better protect medical pros and patients. These important updates took effect on January 16, 2022.
The new law sets clear penalties for those who block healthcare delivery. It’s similar to hate crime legislation that guards vulnerable groups. These rules help ensure everyone can get medical care safely.
These changes tackle the worrying trend of intimidation in healthcare settings. They reassure patients and providers that Canada values its healthcare system. The law aims to keep medical services running smoothly for all.
The Nature of Healthcare Intimidation in Canada
Healthcare workers in Canada face increasing intimidation. This trend threatens their safety and ability to provide care. It creates significant challenges for medical professionals and patients.
Definition and Scope of the Problem
Healthcare harassment includes verbal abuse, threats, and physical aggression towards medical staff and patients. It also involves organized campaigns that disrupt medical services.
These incidents affect healthcare workers’ wellbeing and their ability to deliver quality care. Since 2020, healthcare professionals report more frequent and intense intimidation.
Recent Incidents Across Canadian Provinces
Ontario hospital staff faced aggressive protesters blocking entrances during vaccine rollouts. In British Columbia, workers reported harassment while entering or leaving their workplaces.
Alberta saw demonstrations at medical centers that became intimidating. Ambulances struggled to access emergency departments due to crowds blocking hospital entrances.
Quebec healthcare workers experienced increased verbal aggression from frustrated individuals. These incidents show how public frustration can lead to targeted harassment.
Vulnerable Healthcare Settings
Emergency departments often encounter aggressive behavior from stressed patients or family members. Mental health facilities report higher rates of intimidation due to complex conditions.
Vaccination clinics became targets during the pandemic, facing organized harassment campaigns. Abortion and reproductive health clinics continue to experience targeted intimidation.
Public health offices have become focal points for demonstrations that sometimes escalate. These incidents create unsafe environments for healthcare workers and vulnerable patients.
Intimidation tactics affect staffing levels, service availability, and patient safety. Understanding these patterns is crucial for developing effective protective measures.
Legal Definition of Intimidation to Impede Health Services
Canada’s Criminal Code criminalizes behavior that impedes health services. The law protects healthcare providers and patients. It balances protest rights with uninterrupted access to medical care.
These legal provisions create a framework. They ensure healthcare remains accessible. They also protect the right to peaceful protest.
Section 423.2 of the Canadian Criminal Code
Section 423.2 took effect on January 16, 2022. It addresses harassment of healthcare workers. This amendment responded to incidents during the COVID-19 pandemic.
The law makes it illegal to provoke fear in three scenarios. These include targeting health service seekers, professionals, or their assistants.
- When directed at a person seeking health services
- When targeting a health professional performing their duties
- When aimed at a person assisting a health professional
This comprehensive protection covers all healthcare delivery aspects. It recognizes that intimidation can disrupt critical services. The law also addresses physical obstruction of healthcare facilities.

Elements of the Offense
Several key elements define intimidation to impede health services. First, there must be conduct intended to provoke fear. This can include threats, gestures, or other intimidating behaviors.
Second, the fear must target specific groups. These include healthcare professionals, service seekers, or their assistants. The law protects these vulnerable groups.
Third, the intent must be to disrupt healthcare. This intent requirement separates casual disagreements from criminal acts. Prosecutors must prove the perpetrator meant to impede services.
Distinction from Other Criminal Offenses
This offense differs from general harassment or assault. Section 423.2 focuses on protecting healthcare settings. It distinguishes between legitimate protest and criminal intimidation.
The law allows “obtaining or communicating information” near healthcare facilities. This protects free speech while criminalizing physician intimidation.
| Offense Type | Primary Focus | Maximum Penalty | Context Specificity |
|---|---|---|---|
| Intimidation to Impede Health Services | Healthcare access and delivery | 10 years imprisonment | Specific to healthcare settings |
| General Harassment | Repeated unwanted conduct | 10 years imprisonment | Applies in any context |
| Uttering Threats | Verbal threats of harm | 5 years imprisonment | Applies in any context |
| Assault | Physical harm or threat | 5-14 years (varies by type) | Applies in any context |
The law covers those who assist or attempt such intimidation. This ensures accountability for all participants. It creates a comprehensive framework to protect healthcare delivery.
Statistics and Data on Healthcare Intimidation in Canada
Disturbing trends in healthcare intimidation are emerging across Canada. The Criminal Code was amended to protect healthcare workers after vaccination mandate protests. This change came as evidence highlighted the growing crisis facing medical professionals.
Statistical data began to reveal the extent of the problem. Legislative action became necessary to address the issue. The aim was to safeguard healthcare workers and maintain access to essential services.
National Prevalence Rates
Preliminary findings show a troubling picture of medical staff threats in Canada. About 75% of healthcare workers report experiencing verbal harassment during their careers. One in four face physical threats or violence while working.
These stats reflect a pattern of workplace bullying in healthcare settings. Reception staff and nurses often face the most confrontations. They’re usually the first point of contact with frustrated patients and visitors.

Provincial Variations in Reported Cases
Intimidation incidents vary across Canada’s diverse geography. Urban centers in Ontario and BC report the highest rates. Quebec has seen increases in emergency department confrontations.
Rural healthcare facilities face unique challenges with limited security resources. Alberta and Saskatchewan have experienced protest-related disruptions at healthcare facilities. This has created additional safety concerns for staff.
| Province | Incident Rate (2021) | Most Common Type | Security Resources |
|---|---|---|---|
| Ontario | High (urban centers) | Verbal harassment | Moderate |
| British Columbia | High | Protest disruptions | Moderate to high |
| Quebec | Moderate to high | Emergency dept. incidents | Moderate |
| Alberta | Moderate | Facility protests | Limited (rural areas) |
| Rural regions (all provinces) | Lower reported rate | Individual confrontations | Very limited |
Pandemic-Related Increases in Healthcare Intimidation
The COVID-19 pandemic marked a turning point in medical staff threats across Canada. Between 2019 and 2021, reported intimidation incidents increased by 35-50% nationwide. This surge coincided with tensions around vaccination policies and mask mandates.
Online harassment of healthcare workers also rose dramatically. Physicians report receiving threats through social media and email. This extends the reach of intimidation beyond physical workplace settings.
COVID-19 Impact on Healthcare Worker Safety
Frontline workers report unprecedented stress during the pandemic era. This stress comes from clinical duties and confrontations with patients and the public. Nurses and reception staff face the highest rates of verbal abuse.
The pandemic has worsened workplace bullying in healthcare environments. Staff shortages and increased workloads have created pressure-cooker conditions. These factors explain why legislative protection became necessary for healthcare workers.
Common Forms of Intimidation to Impede Health Services
Canadian healthcare facilities face various forms of intimidation that compromise emergency room safety. These behaviors range from verbal confrontations to organized disruptions. Understanding these challenges helps facilities develop prevention strategies and response protocols.
Verbal Threats and Harassment
Verbal intimidation is the most common form of harassment in healthcare settings. It includes raised voices, profanity, and explicit threats directed at staff members. Reception desks and triage areas often become hotspots for these incidents.
Verbal harassment often escalates when patients or visitors feel their needs aren’t met quickly enough. Healthcare workers report being called names, receiving threats, and enduring repeated abuse during shifts. These interactions create a hostile work environment and cause psychological distress among staff.
Physical Intimidation and Violence
Physical intimidation poses the most immediate threat to hospital safety. It includes aggressive gestures, invasion of personal space, throwing objects, and direct assaults on healthcare workers. Emergency departments face high risks, with nurses and security personnel often targeted.

Patients under the influence of substances or experiencing mental health crises often cause physical violence. Family members of patients also contribute to these incidents, especially during high-stress situations. Dissatisfaction with care can lead to aggressive behavior from visitors.
Cyberbullying and Online Harassment
The digital age has introduced new ways to intimidate healthcare workers. Cyberbullying includes targeted campaigns against providers on social media and negative online reviews with personal attacks. Doxxing, or publishing private information about healthcare workers, is another form of online harassment.
This form of intimidation gained prominence during the COVID-19 pandemic. Healthcare professionals advocating for public health measures faced organized online harassment. Cyberbullying can be particularly severe as it follows workers into their personal lives.
Protest-Related Disruptions at Healthcare Facilities
Recent years have seen an increase in organized protests targeting healthcare facilities. These demonstrations sometimes block entrances, use loud sounds to disrupt services, or confront workers. Some protesters display graphic imagery to intimidate staff and patients.
Canadian law protects legitimate protest, but actions that impede care or create fear are criminal intimidation. Section 423.2 of the Criminal Code addresses behaviors that interfere with healthcare delivery. Facilities must balance free speech rights with ensuring safe access to medical care.
| Form of Intimidation | Common Locations | Primary Targets | Impact on Emergency Room Safety |
|---|---|---|---|
| Verbal Harassment | Reception, Triage, Patient Rooms | Nurses, Receptionists | Moderate – Creates hostile environment |
| Physical Violence | Emergency Department, Psychiatric Units | Nurses, Security Staff | Severe – Direct safety threat |
| Cyberbullying | Online Platforms, Social Media | Physicians, Public Health Officials | Indirect – Staff retention issues |
| Protest Disruptions | Facility Entrances, Parking Areas | All Staff, Patients | High – Delays emergency access |
Legal Consequences for Perpetrators in Canada
Canada’s legal system harshly punishes those who intimidate healthcare workers. Federal and provincial laws protect nursing staff and essential health services. These consequences matter for both healthcare workers and the public.
Criminal Penalties and Sentencing Guidelines
The Criminal Code of Canada sets strict penalties for healthcare intimidation. Indictable offenses can lead to 10 years in prison. Summary convictions may result in up to two years less a day.
Judges consider several factors when sentencing offenders. These include targeting health service providers or blocking access to care. The intimidation’s severity and service disruptions also affect sentencing decisions.

Notable Canadian Case Precedents
Since 2022, cases of healthcare intimidation have shaped legal precedents across Canada. Courts take these offenses seriously, especially when services are disrupted or behavior is repeated.
These cases help establish consistent law interpretation and sentencing ranges. They also show that intimidating healthcare workers won’t be tolerated in Canada.
Provincial Variations in Enforcement
Canadian provinces enforce these laws differently. Ontario and British Columbia have created special teams for healthcare facility disturbances. Other provinces are still developing their enforcement strategies.
These differences reflect unique regional challenges and evolving approaches. As more cases progress, expect more consistent nationwide law application.
Enhanced Penalties in Specific Jurisdictions
Some provinces have added measures beyond federal laws. Quebec has administrative penalties for healthcare facility disruptions. British Columbia has “access zones” with extra restrictions around certain facilities.
Alberta has protocols for quick response to healthcare disturbances. These provincial measures strengthen federal protections for healthcare workers and patients.
Reporting Procedures for Healthcare Intimidation Incidents
Proper reporting of healthcare intimidation incidents is vital for protecting medical staff and maintaining clinic security. Established procedures ensure incidents are documented, addressed, and potentially prosecuted. These protocols form the basis of healthcare facility safety and create a safer environment.
Immediate Response Protocols
Safety is the top priority when intimidation occurs. Effective immediate response protocols include de-escalation techniques and clear communication channels for assistance.
They also involve predetermined security responses and safe zones for staff retreat. Regular practice ensures all staff know how to handle threatening situations.
Documentation Requirements
Thorough documentation is essential for both safety and legal protection. Incident reports should include date, time, location, and names of those involved.
They should also detail threatening behaviors, verbatim threats, witness information, and actions taken. Preserve any photo or video evidence that might help identify perpetrators or clarify the incident.
Institutional Reporting Channels
Healthcare facilities have specific channels for reporting intimidation incidents. These include standardized forms, safety officers, and occupational health departments for staff support.
Anonymous reporting options are available for staff fearing retaliation. Reports should flow through supervisors to administration and external authorities when appropriate.
Law Enforcement Collaboration
Severe intimidation incidents require law enforcement involvement. Recent Criminal Code amendments have enhanced police investigative tools for serious cases.
“The recent amendments enable law enforcement to obtain an order from a judge to intercept private communications when investigating instances of intimidation against health-care professionals, provided specific safeguards contained in the Criminal Code are met.”
Effective collaboration with law enforcement includes establishing healthcare-familiar contacts and developing rapid response protocols. Joint training exercises also improve preparedness for healthcare facility incidents.
Impact on Canadian Healthcare System and Workers
Intimidation in healthcare settings causes widespread damage to Canada’s medical system. It affects more than just individuals. It impacts hospital operations, patient care, and healthcare sustainability nationwide. Understanding these effects is key to developing solutions.
The consequences reach far beyond the targeted people. They touch every aspect of healthcare delivery. This makes it a pressing issue for the entire medical community.
Psychological Effects on Healthcare Professionals
Healthcare workers facing intimidation often suffer severe mental distress. Up to 60% of medical staff experiencing workplace bullying in healthcare report anxiety, depression, and burnout symptoms.
About 25% of affected staff seek professional mental health help. Many need extended time off work. This impacts their job satisfaction and clinical decision-making confidence.
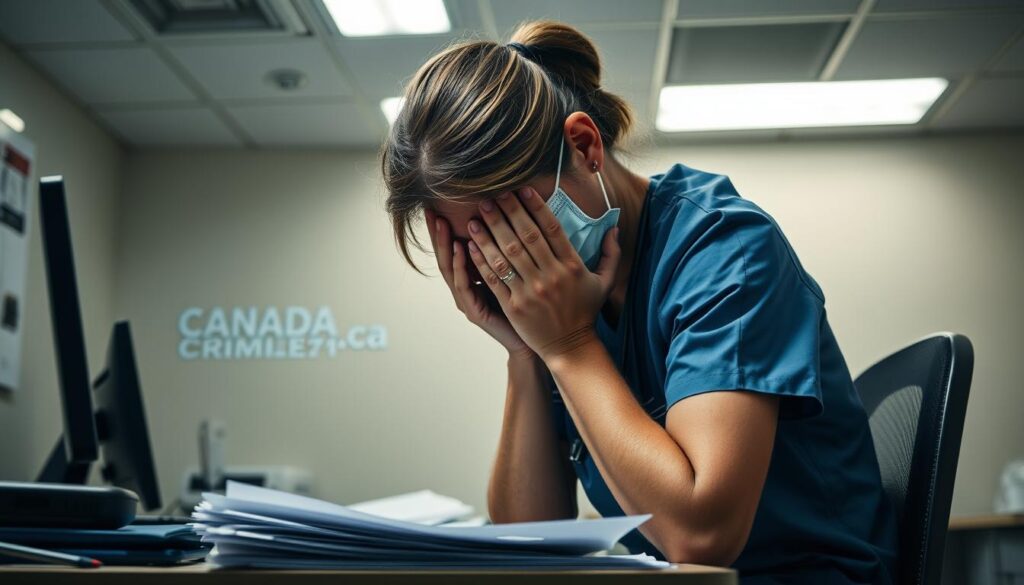
A 2022 survey revealed alarming results. 68% of Canadian nurses considered quitting due to hostile work environments. This shows how physician intimidation directly threatens workforce stability.
Staff Retention and Recruitment Challenges
Canada’s healthcare sector already faces significant staffing shortages. Intimidation makes this problem much worse. Safety concerns are now a top reason medical professionals leave their jobs.
Rural healthcare facilities face severe challenges. In small towns, medical staff are easily identified. This makes them more vulnerable to targeted intimidation.
Recruitment efforts suffer too. Medical students increasingly avoid high-risk specialties or facilities known for security issues.
Service Disruptions and Patient Care Implications
Intimidation often leads to immediate healthcare service disruptions. Emergency department closures due to staff safety concerns have risen 35% since 2020.
Even when facilities stay open, patient care suffers. Units with high workplace bullying in healthcare rates show 28% more medication errors.
Many patients delay seeking care when they feel healthcare facilities are unsafe. This leads to more complex medical issues and poorer outcomes.
Economic Costs to the Healthcare System
Healthcare intimidation costs Canada’s medical system heavily. Direct costs include increased security, worker compensation claims, and sick leave coverage.
Indirect costs are even higher. These include recruitment, training for new staff, reduced efficiency, and legal proceedings related to physician intimidation.
| Impact Category | Estimated Annual Cost | Percentage of Healthcare Budget | Trend Since 2020 |
|---|---|---|---|
| Staff Replacement | $175 million | 0.8% | Increasing (+22%) |
| Security Enhancements | $120 million | 0.5% | Increasing (+45%) |
| Sick Leave/Disability | $210 million | 0.9% | Increasing (+18%) |
| Legal Proceedings | $85 million | 0.4% | Increasing (+30%) |
Workplace violence and intimidation cost the Canadian healthcare system over $590 million yearly. This money could support patient care, improve facilities, or address staffing shortages.
These impacts show why addressing intimidation is crucial for public health. It’s a key challenge for healthcare sustainability in Canada. Without action, these problems could weaken the nation’s entire healthcare system.
Protective Measures and Prevention Strategies
Protecting healthcare workers requires physical, procedural, and technological measures. The government aims to safeguard staff while respecting peaceful protest rights. Effective strategies reduce incidents and create a secure atmosphere for everyone.
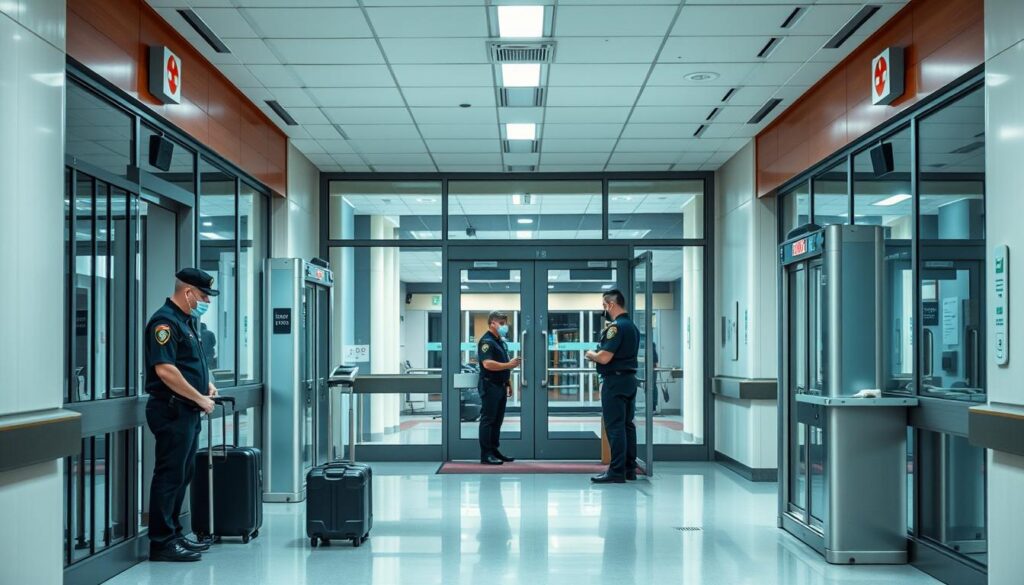
Institutional Security Protocols
Canadian healthcare facilities have implemented comprehensive security protocols. These include controlled access systems and clear visitor policies. Many have installed panic buttons in high-risk areas.
Strategic security personnel deployment focuses resources where needed most. Environmental design improvements enhance visibility and reduce isolated areas. Color-coded alert systems quickly communicate threat levels without alarming patients.
De-escalation Training Programs
De-escalation training is a powerful tool against clinic security risks. It teaches staff to recognize early warning signs of aggression. Workers learn techniques to defuse tense situations safely.
Training covers safe positioning and knowing when to seek help. Facilities with comprehensive training see 25-60% reductions in violent incidents. This shows the value of investing in staff preparation.
Alberta’s workplace violence prevention resources offer guidance on developing effective healthcare training programs.
Technological Solutions for Enhanced Safety
Modern tech offers tools to boost healthcare facility security. Personal alarms allow quick calls for help. Video monitoring deters incidents and provides evidence.
Electronic access controls restrict unauthorized entry. Advanced communication systems enable discrete assistance calls. Some facilities use mobile apps for staff to alert security quickly.
Provincial Healthcare Security Initiatives
Canadian provinces have developed specialized healthcare security approaches. These initiatives address regional needs while sharing common protection goals.
| Province | Initiative | Key Features | Implementation Status |
|---|---|---|---|
| British Columbia | Violence Prevention Program | Standardized protocols across health authorities | Fully implemented |
| Ontario | Workplace Violence Prevention in Health Care Leadership Table | Sector-specific recommendations and resources | Ongoing implementation |
| Alberta | Healthcare Worker Identification System | Province-wide incident tracking across facilities | Fully implemented |
| Quebec | Specialized Response Teams | Dedicated units for high-risk healthcare environments | Pilot program expanding |
Effective prevention combines physical security, staff training, clear policies, and a supportive culture. This approach creates an environment focused on health and healing. It allows providers and patients to prioritize what matters most.
Conclusion: Safeguarding Canadian Healthcare Services
Canada’s healthcare services need a balanced approach to address patient safety concerns. The 2022 Criminal Code amendments create specific offences to protect healthcare workers and patients. These legal changes establish clearer boundaries for those who obstruct access to health services.
When visiting an emergency room in Canada, you now have additional legal protections. These ensure your right to receive care without interference. The new laws take effect 30 days after receiving Royal Assent.
Several priorities emerge for strengthening these protections. Consistent application of laws across provinces is crucial. Developing better tracking systems to identify intimidation patterns is also important. Investing in security measures to enhance emergency room safety is essential.
The success of these measures relies on collaboration between healthcare facilities and law enforcement. Government agencies also play a key role. Legal consequences are necessary, but fostering respect for healthcare professionals is equally vital.
This comprehensive approach will make the healthcare system safer for all Canadians. It’s about preserving one of Canada’s most essential public resources. Everyone should be able to access care when they need it most.

